Osteoarthritis of the knee is a degenerative condition in which the cartilage in your joint slowly breaks down. It’s the most common type of arthritis that affects your knee joint. OA is a lifelong, progressive condition, but treatment can help manage your symptoms. When it becomes severe, your provider might recommend knee replacement surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
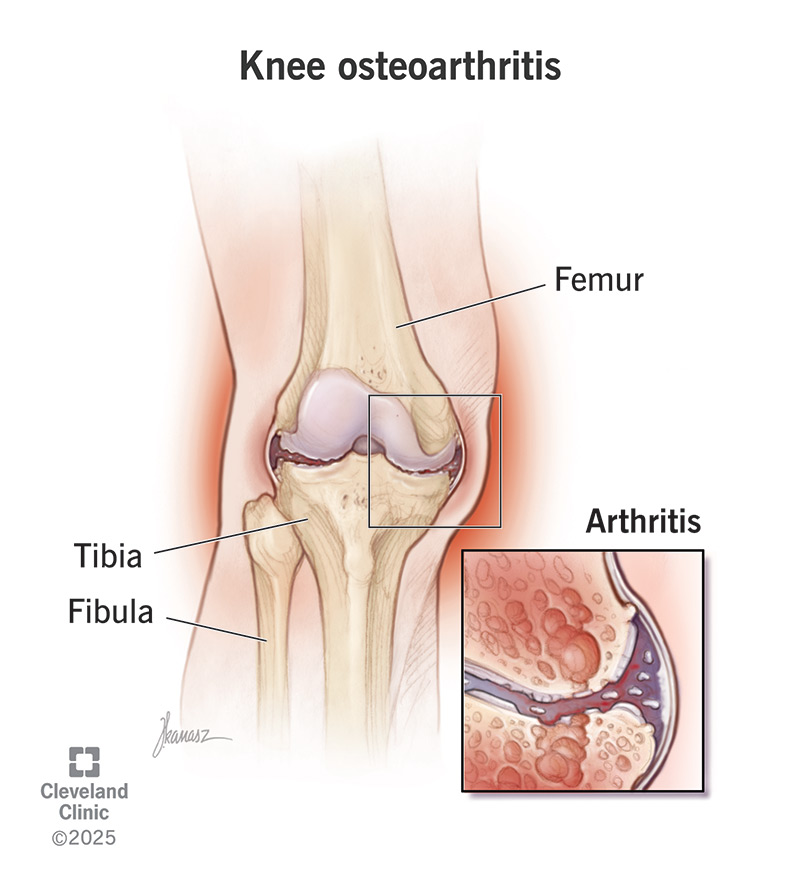
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/knee-osteoarthritis)
Osteoarthritis of the knee happens when the cartilage in your knee joint breaks down, causing the bones to rub together. This friction causes pain and swelling in your knee, leading to stiffness. Osteoarthritis is a degenerative joint disease — a product of wear and tear over time. It’s very common, and the knee, which takes a lot of stress over your lifetime, is one of the most common joints affected.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Osteoarthritis (OA) in your knee is a long-term, progressive condition with no cure. There are many treatments available to slow its progress and ease your symptoms, and lifestyle changes can help. But it does tend to worsen with time, and it can eventually lead to disability. Your healthcare provider will monitor your arthritis as it progresses. When it starts to really impact your life, surgery is an option.
While there aren’t definitive stages of osteoarthritis in your knee, it is a degenerative condition that progresses in a predictable way. (This is different from other types of arthritis in your knee.) Your healthcare provider might use stages or levels to explain how advanced your condition is. Understanding how osteoarthritis progresses can help you understand your symptoms and what to expect next.
Stages include:
Advertisement
Knee pain is the most common symptom of knee osteoarthritis. Your knee might hurt when you put pressure on it, when you move it or even when you’re sitting still. Other OA knee symptoms include:
As knee arthritis progresses, it can cause some additional negative side effects, including:
Osteoarthritis of the knee happens when the cartilage in your knee joint wears down. Cartilage covers the ends of your bones where they meet in your knee joint. It provides padding that allows the bones to move smoothly against each other. It also absorbs shock when you put weight on your knee. When cartilage breaks down, it can’t grow back. As you lose it, you start to lose mobility in your joint.
OA is usually just the result of gradual wear and tear on your joint over time. Sometimes secondary factors, like an injury or extra stress on your knees, contribute to wearing them down sooner. The cartilage in your knees is like your car’s shock absorber, protecting your car from bumps and jolts. If you drive on rough roads, your shocks wear out faster. If you drive on smooth roads, your shocks last longer.
You might be more likely to develop OA in your knee if:
Your healthcare provider will start by asking about your symptoms and physically examining your knee. They’ll check:
Advertisement
They’ll follow up with imaging tests. Usually, a knee X-ray will show evidence of knee osteoarthritis. In some cases, they might order an MRI or CT scan if they need to look more closely at tissues in your joint.
Knee osteoarthritis treatments include lifestyle changes, nonsurgical treatments and surgery. Typically, healthcare providers try nonsurgical treatments first before recommending surgery for knee OA.
Nonsurgical osteoarthritis of the knee treatments include:
Surgical osteoarthritis of the knee treatments include:
Advertisement
Since there’s usually no single cause of knee osteoarthritis, you can’t entirely prevent it. But you can reduce your risk by reducing stress and strain on your knee joint where possible. For example:
Osteoarthritis of the knee develops over time. You might not notice the twinge or ache that could be the first sign of knee osteoarthritis until it worsens. Talk to your healthcare provider if you’ve recently developed knee pain for no apparent reason, and it seems to be getting worse. Early treatment offers the best chance of slowing down osteoarthritis and managing your symptoms without surgery.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Stiff, painful joints can make daily life challenging. Cleveland Clinic orthopaedic specialists can help you find relief from osteoarthritis and get you moving again.
